GRECC Connect Program Site - Pittsburgh, PA
Michelle Rossi, MD, MPH is a Board Certified Geriatrician at the VA Pittsburgh Healthcare System (VAPHS). She is the Associate Director for Clinical Care at the Pittsburgh VA GRECC. She also is the Medical Director for the Geriatric Evaluation and Management Clinic, VAPHS Geriatric Driving Safety Clinic; VAPHS Dementia Clinic; the Geriatric Polypharmacy E-consult, and VAPHS TeleDEMENTIA clinic (CVT). She works with Geriatric Workforce Enhancement Project (GWEP). Dr. Rossi is the recipient of the Federal Executive Board 2013 Outstanding Team Award for VAPHS CVT TeleDEMENTIA and the Federal Executive Board 2015 in the Outstanding Professional Employee-Medical/ Scientific Category. She also received a University of Pittsburgh Medical Center award for Excellence in Patient Experience in 2016.
Stacey Shaffer, MD is a Board Certified Geriatrician at the VA Pittsburgh Healthcare System. Dr. Shaffer has worked with the VAPHS GRECC, home-based primary care, and the Geriatric Polypharmacy E-Consult service. Currently, she provides care for veterans with dementia via CVT TeleDEMENTIA program, and she assists with the VAPHS CVT Dementia Caregiver Support group.
Carol Dolbee, CRNP is a Nurse Practitioner at the VA Pittsburgh Healthcare System. She joined the VA in 2001. She is part of the clinic staff in the Geriatric Evaluation and Management (GEM) clinic, Dementia Clinic, Geriatric Driving Safety Clinic, and TeleDEMENTIA clinic. Also, she contributes care of older veterans through the VAPHS GRECC Geriatric Polypharmacy Consult service, and The Program for Intensive Residential Aphasia Treatment and Education (PIRATE). Mrs. Dolbee is the recipient of the FEB 2013 Outstanding Team Award for VAPHS CVT TeleDEMENTIA.
Nancy Kovell, LCSW is a Social Worker at VA Pittsburgh Healthcare System with over 20 years of medical social work experience including clinical experience with the University of Pittsburgh Medical Center. She is extensively knowledgeable of clinical social work practices and interventions with both adult and geriatric populations and their caregivers. Besides her contribution to the TeleDEMENTIA , Mrs. Kovell has been instrumental in addressing the needs of Caregiver stress through the Geriatric Workforce Enhancement Project. Mrs. Kovell is the receipient of the FEB 2013 Outstanding Team Award for VAPHS CVT TeleDEMENTIA
Paul Bulgarelli, DO is the Chief of consultation/Liaison Psychiatry at VA Pittsburgh Healthcare System. He has been on staff at VAPHS since 2003, after finishing a Geriatric Psychiatry Fellowship at Western Psychiatric Institute and Clinic at University of Pittsburgh Medical Center. He is board certified in both general adult and geriatric psychiatry. Interests include medical psychiatry, consultation psychiatry and emergency psychiatry. Dr. Bulgarelli is the recipient of the the FEB 2013 Outstanding Team Award for VAPHS CVT TeleDEMENTIA
Lauren Jost, PsyD is a clinical psychologist at VA Pittsburgh Healthcare System. She works in the Geriatric Evaluation and Management Clinic and in Primary Care Mental Health Integration. Her doctoral training included an emphasis in Geropsychology, and she received specialized training in geriatrics as part of her Geropsychology post-doctoral fellowship. She is also a Geriatrics Scholar and completed her training at the Palo Alto VAMC. Other clinical experiences include working with older adults in the VA’s Community Living Center and Home-Based Primary Care. Besides her contribution to the TeleDEMENTIA psychological assessment, Dr. Jost also addresses the needs of Caregiver stress through the TeleDEMENTIA Caregiver Support Group.
POC: Ina Engel, Ina.Engel@va.gov; (412) 360-2919
A TeleDEMENTIA CVT Caregiver Support Group was begun in 2016 with service to 5 CBOC’s. The TeleDEMENTIA clinic success was recognized: in 2014, when the TeleDEMENTIA team was awarded a Pittsburgh Federal Executive Board Excellence in Government bronze team award. In 2016, the TeleDEMENTIA Clinic was awarded a semi-finalist award in the Under Secretary of Health’s Promising Practice initiative. This clinic is being used as a model for a number of other programs in development.
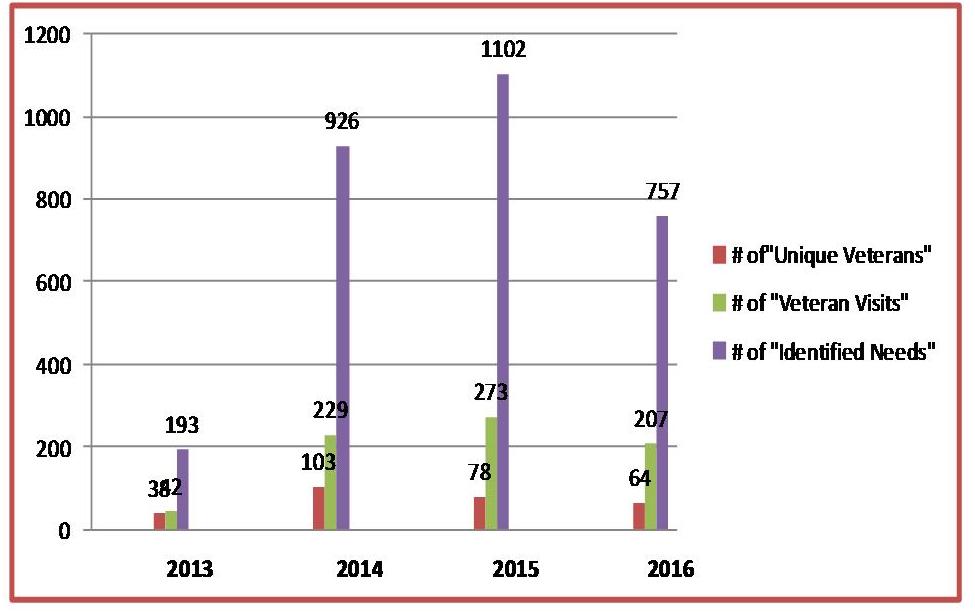
HIGHLIGHTSThe TeleDEMENTIA Clinic at the Veterans Administration Pittsburgh Healthcare System (VAPHS) has grown dramatically since its inception in Fiscal Year 2013. Not only has an actual increase in the number of evaluations continued to occur, but identifying the needs of this Veteran population has also been more aggressively addressed.
A Veteran referred to the TeleDEMENTIA Clinic is evaluated by a team of medical providers: Geriatric Medical Physician, Nurse Practitioner, Geriatric psychiatrist, psychologist, and social workers who work together as progressive same day appointments. Often this eliminates the need for the Veteran to make more than one visit to the Community Based Outpatient Clinic (CBOC). It saves the Veteran and their caregiver time, miles driving, additional copays, and the added burden on already overstressed caregivers. The team sees Veterans with suspected or known cognitive decline and can determine diagnoses.
- The team addresses changing needs of the Veteran over time including: depression, agitation, confusion, driving concerns, respite, medication, nutrition, balance and gait.
- The team educates the Veteran and the caregiver about VA services as well as local and county services that maybe helpful to the Veteran.
This following graph reflects the VAPHS CVT TeleDEMENTIA yearly growth. The number of Unique Veterans, Veteran visits and Identified needs.
POSTER:
Gerontological Society of America Annual meeting, November, 2013 New Orleans. “Clinical Video Telehealth for Dementia Assessment: Creation of TeleDEMENTIA Clinic.”
American Geriatric Society Annual Meeting, May 2014, Orlando, FL. “Dementia Treatment with Clinical Video Telehealth”
American Geriatric Society Annual Meeting, May 2014, Orlando, FL. “Improving Patient and Caregiver Satisfaction in a TeleDEMENTIA Clinic”
IAGG: San Francisco July, 2017: Clinical Video Telehealth (CVT) for Dementia: Rural Provider & Veteran Recommendations
SYMPOSIA:
Gerontological Society of America Annual Meeting, November, 2014 Washington, DC “TeleDEMENTIA Clinic: Clinical Video Telehealth to Diagnose and Support Rural Veterans With Dementia”
Gerontological Society of America Annual Meeting, November , 2015 Orlando, FL “Interprofessional TeleDEMENTIA Clinic: Findings the First Year”
PUBLICATIONS:
Powers BB, Homer MC, Morone N, Edmonds N, Rossi MI..Creation of an Interprofessional Teledementia Clinic for Rural Veterans: Preliminary Data. J Am Geriatr Soc. 2017 May;65(5):1092-1099. doi: 10.1111/jgs.14839. Epub 2017 Mar 10.
REGIONAL PRESENTATIONS:
VA Rural Interdisciplinary Team Training program (RITT) programs provided to:
- May 20, 2013, M. Rossi, MD, MPH, Coatesville Home Based Primary Care team, Coatesville VAMC, Coatesville, PA
- May 2, 2014, M. Rossi, MD, MPH, Tucker county CBOC, M. Rossi, MD, MPH Parsons, WV
- April 23-24, 2015, M. Rossi, MPH, Lancaster CBOC, Lancaster, OH & M. Rossi, MD, MPH, Portsmouth CBOC, Portsmouth, OH
- July 28-29, 2016, M. Rossi, MD, MPH, Marietta CBOC, Marietta, OH & M. Rossi, MD, MPH, Athens CBOC, Athens, OH
March 15, 2016: M. Rossi, MD, MPH “GeriPACT and TeleHealth”, GeriPACT Summit, Albany , NY
September 26, 2014: B. Brott, MD : Multidisciplinary Team Approach to Creating a TeleDEMENTIA Clinic. GRECC Lecture Series, VAPHS, Pittsburgh, PA
March 17, 2016 : M. Rossi, MD, MPH: TeleDEMENTIA Clinic and its outcomes from the past 3 years. Division of Geriatric Medicine Conference, University of Pittsburgh Medical Center, Pittsburgh, PA
GRECC ADVISORY COMMITTEE presentations
- May 23, 2013, M. Rossi, MD, MPH: TeleDEMENTIA
- February 25, 2014 M. Rossi, MD, MPH: TeleDEMENTIA
AWARDS
2013 - Outstanding Team Award for VAPHS CVT TeleDEMENTIA Team
2015 - M. Rossi, MD, MPH recipient of the Outstanding Professional Employee-Medical/ Scientific Category.
2016 - TeleDEMENTIA Clinic was awarded a semi-finalist award in the Under Secretary of Health’s Promising Practice Initiative in two 2016 competitions.
Geriatric Workforce Enhancement Project (GWEP)
- Caregiver Support Group: provides education and support to caregivers of elderly Veterans with dementia who receive primary care though the CBOCs via monthly meetings through teleconferencing.
Geriatric Polypharmacy E consults
- Focus on the critical problem of inappropriate medication prescribing and use among older rural Veterans especially those with a most complex medication regimen. The goal being a simpler regimen that is cost effective yet efficacious and which minimizes side effects for the older adult.
Geriatric Evaluation and Management Clinic (GEM)
- Specialized program of services in an outpatient setting performed by an interdisciplinary health care team for Veterans who would most likely remain in an independent environment. The evaluation includes rehabilitation, health promotion and social service intervention.
Geriatric Driving Safety Clinic (GDSC)
- Evaluation of the elderly Veteran driver as an outpatient is performed by an interdisciplinary health care team based on the recommendations provided by the American Medical Association in agreement with the Commonwealth of Pennsylvania.
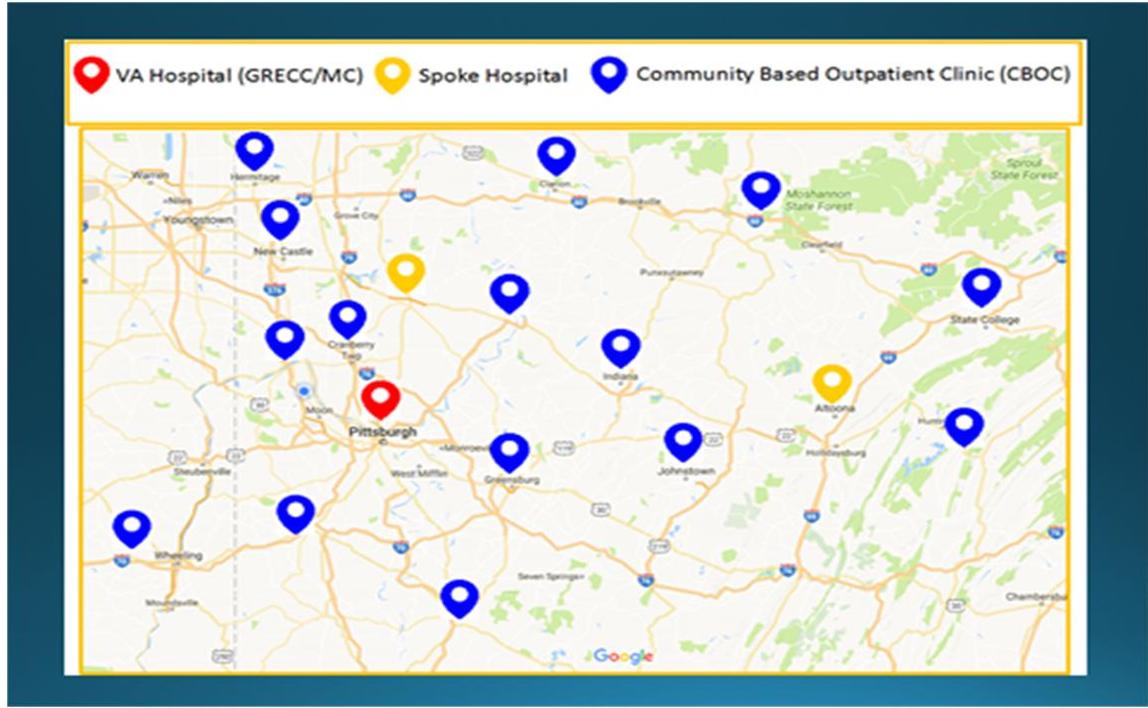
VA GRECC/MC
VA Pittsburgh Healthcare System
SPOKE HOSPITALS
ALTOONA: James E. Van Zandt VA Medical Center
BUTLER: VA Butler Healthcare
CBOCs
Armstrong/ Kittanning, PA Beaver/ Monaca, PA
Belmont/ St. Clairsville, OH Clarion/ Monroe Twp., PA
Cranberry/ Cranberry Twp., PA DuBois
Fayette/ Uniontown, PA Huntingdon/ Mapleton Depot, PA
Indiana Johnstown
Lawrence/ New Castle, PA Mercer/ Hermitage, PA
State College Washington
Westmoreland/ Greensburg, PA